Patellofemoral Pain
Patellofemoral Pain Syndrome (referred to as Chrondromalacia Patella or Anterior Knee Pain Syndrome or Runner’s Knee in the past) is a condition where pain is felt behind or around the patella, specifically when doing activities that compress the patellofemoral joint like running, jumping, climbing stairs, and squatting (aka loading while flexed). Both the shape of the patella (kneecap) and weak abductors can be associated with this syndrome. (1)
When diagnosing PFPS the issue is that orthopedic testing is very subtle at times, and doesn’t always correlate with pain felt during activity. Findings during examination should contribute to the plan of care for each patient.
A 2012 Systematic review looking at the risk factors of PFPS found that a weak quadriceps muscle increased risk, likely due to patellar instability. (2)
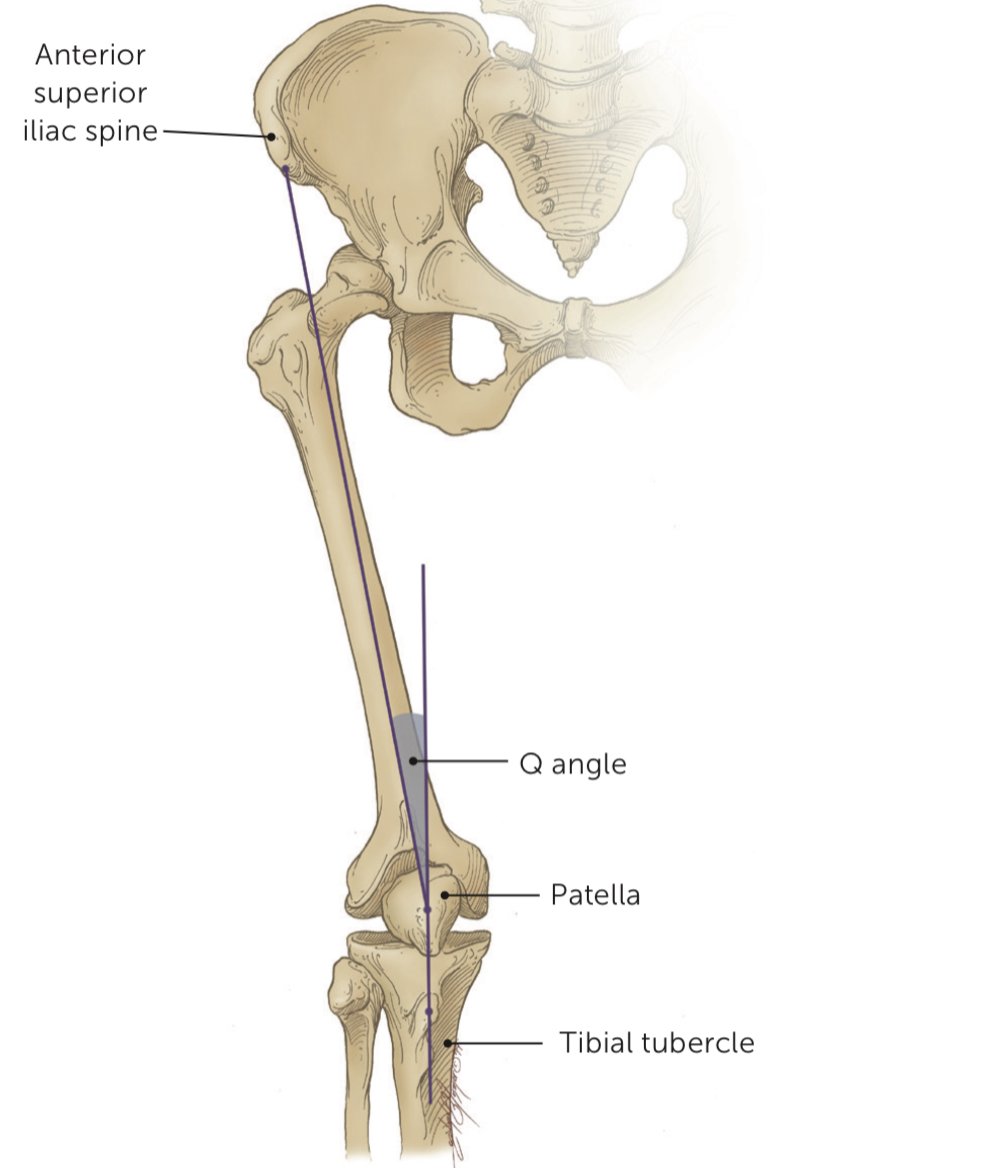
The Q angle (the angle made between the line that ASIS and centre of patella with the line that is made between centre of patella and middle of tibial tuberosity) has been thought to be related to potential PFPS. The greater the Q angle the greater the tendency for the patella to migrate laterally when the quadriceps is activated. This is still demonstrated in recent literature, but the Q angle must be measured with the standardized protocol. (1)
Q Angle
Patellar tilt (specifically laterally) has been said to also indicate PFPS, but analysis of research found that “statistical values did not represent clear evidence” (1).
Crepitus can or cannot be associated with PFPS. We do know that “knee crepitus had no relationship with self-reported clinical outcomes of women with PFPS”. (1)
Although studies in the past have found patients with PFPS to have muscle weakness in abduction of the hip, extension of the knee and external rotation of the hip, testing is unreliable. Instead functional testing should include “anteromedial lunge, stepdown, single-leg press, bilateral squat, and balance and reach”. (1)
When looking at the 2022 Systematic Review looking at squatting risks with PFPS, it seems that all squatting causes tension overload on the patellofemoral joint, more specifically in the 60-90 deg knee flexion range. The main cause of worsening knee pain during squatting seems to be translation of the knee over the toes during squatting and muscle imbalance in the thigh. (3)
Another study that divided participants into two groups, one with just quadriceps/hamstring strengthening and gastroc/hamstring/glute stretching and the other with added core training. They found the addition of core training to improve functional outcomes even greater than just knee exercises. (4)
When looking into the impact foot and ankle alignment has on PFPS, the evidence is inconclusive and conflicting due to poor quality. (5)
Exercise is recommended but should be tailored to each patient based on examination. A mix of core, flexibility, and strength training should be prescribed, 3 times per week for 6 to 8 weeks. Orthotics may be used in combination with exercise. The same goes for taping, which may be more beneficial earlier on, although the research is not clear as far as taping is concerned. (6)
In a 2011 study, VMO exercise combining quad strengthening with adductor activation (wall sit combined with ball on back for squatting and ball between knees for adductors) found improved strength and function with patients with PFPS although no change in pain or range of motion was seen. (7)
REFERENCE LIST:
Kasitinon D, Li WX, Wang EX, Fredericson M. Physical examination and patellofemoral pain syndrome: an updated review. Current reviews in musculoskeletal medicine. 2021 Oct 29:1-7.
Lankhorst NE, Bierma-Zeinstra SM, van Middelkoop M. Risk factors for patellofemoral pain syndrome: a system- atic review. J Orthop Sports Phys Ther. 2012;42(2):81-94.
Pereira PM, Baptista JS, Conceição F, Duarte J, Ferraz J, Costa JT. Patellofemoral Pain Syndrome Risk Associated with Squats: A Systematic Review. International Journal of Environmental Research and Public Health. 2022 Jul 28;19(15):9241.
Kasitinon D, Li WX, Wang EX, Fredericson M. Physical examination and patellofemoral pain syndrome: an updated review. Current reviews in musculoskeletal medicine. 2021 Oct 29:1-7.
Martinelli N, Bergamini AN, Burssens A, Toschi F, Kerkhoffs GM, Victor J, Sansone V. Does the Foot and Ankle Alignment Impact the Patellofemoral Pain Syndrome? A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2022 Apr 17;11(8):2245.
Gaitonde DY, Ericksen A, Robbins RC. Patellofemoral pain syndrome. American family physician. 2019 Jan 15;99(2):88-94.
Chaudhari LD, Rao K. Effectiveness of General Quadriceps strengthening versus selective Vastus Medialis Obliquus strengthening in Patellofemoral Pain Syndrome. IJBAMR. 2011 Dec;1(1):71-6.